Introduction to GLP-1 and Its Biological Role
Glucagon-Like Peptide 1 (GLP-1) is a hormone primarily produced in the intestinal L-cells in response to food intake. Its significance in the human body arises from its multifaceted role in regulating glucose metabolism and promoting overall metabolic health. One of the main functions of GLP-1 is to stimulate insulin secretion, a process that is essential in reducing blood glucose levels after meals. At the same time, GLP-1 inhibits the release of glucagon, another hormone that typically raises blood glucose levels by promoting glycogen breakdown in the liver.
Additionally, GLP-1 plays a crucial role in slowing gastric emptying. By delaying the passage of food from the stomach to the small intestine, it ensures a gradual and steady rise in blood glucose levels, preventing sharp spikes. This action not only contributes to better glucose control but also promotes a feeling of fullness or satiety. This enhanced satiety effect can be particularly beneficial in managing body weight, as it reduces overall food intake, thereby influencing calorie balance and energy homeostasis.
Given these mechanisms, GLP-1 is of particular interest in the context of diabetes management. For individuals with type 2 diabetes, GLP-1-based therapies aim to mimic or enhance the hormone’s natural actions, thereby aiding in the effective regulation of blood glucose levels. This integration of pharmacological strategies with GLP-1’s biological functions represents a promising avenue for improved glycemic control.
The secretion of GLP-1 in response to food intake underlines its natural role in postprandial glucose regulation. The intricate interplay between GLP-1 secretion and dietary habits underscores the importance of diet in metabolic health. Understanding GLP-1’s functions provides valuable insight into developing dietary and therapeutic approaches to enhance metabolic outcomes, especially for individuals managing conditions like diabetes.
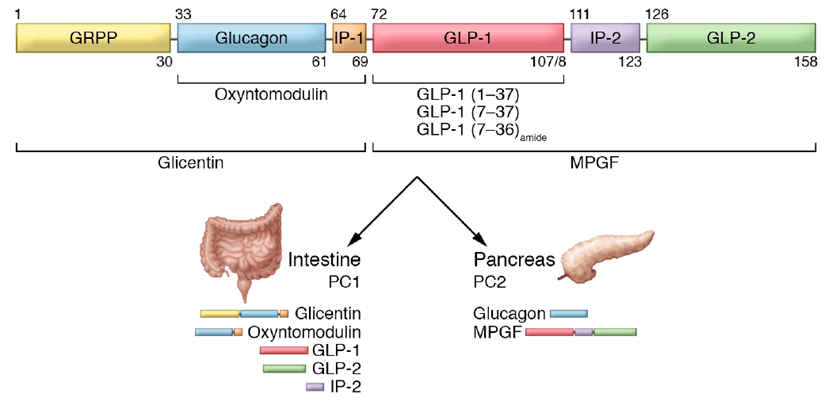
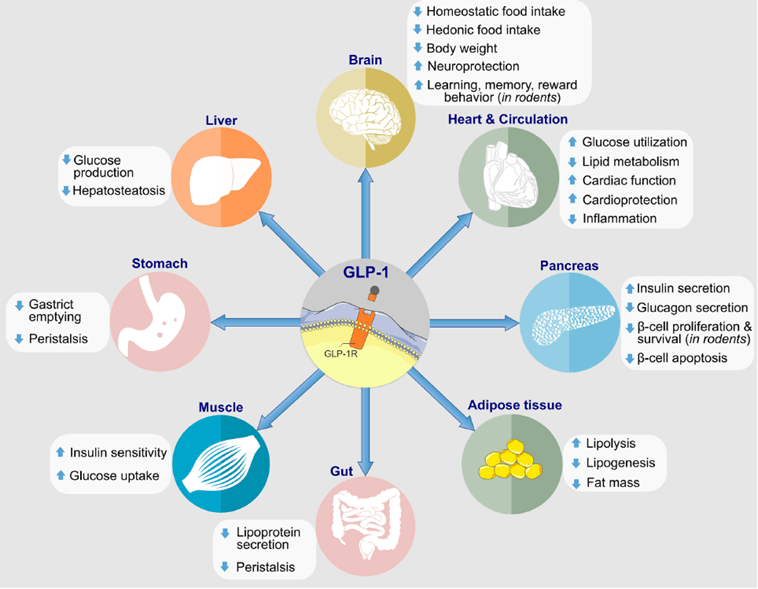
The Mechanism of GLP-1 in the Body
Glucagon-like peptide-1 (GLP-1) functions primarily through its interaction with specific receptors known as GLP-1 receptors (GLP-1R) distributed in diverse tissues including the pancreas, brain, and gastrointestinal tract. Upon binding to GLP-1R, a complex cascade of signaling pathways is initiated, yielding various physiological effects. In the pancreas, GLP-1 promotes insulin release from beta cells, a process essential for lowering blood glucose levels. This action is mediated by the cyclic AMP (cAMP) signaling pathway, which amplifies insulin secretion in response to food intake.
Moreover, GLP-1 reduces the secretion of glucagon from alpha cells in the pancreas. Glucagon is a hormone that typically raises blood glucose levels by stimulating glucose production in the liver. By inhibiting glucagon release, GLP-1 prevents unnecessary glucose output, thus aiding in blood glucose regulation.
The gastrointestinal tract also plays a significant role in GLP-1 activity. It enhances the functionality of the gut-brain axis by promoting satiety signals to the brain, thus helping to regulate appetite. Through neural pathways, especially within the hypothalamus and brainstem, GLP-1R activation results in decreased food intake and prolonged feelings of fullness, contributing to dietary management.
In addition to its metabolic roles, GLP-1 exhibits neuroprotective properties in the central nervous system. Studies indicate that GLP-1 signaling can potentially preserve neuronal health and function, aiding in conditions like Alzheimer’s disease and other neurodegenerative disorders. This neuroprotection is thought to be linked with anti-inflammatory processes and inhibition of neuronal apoptosis, emphasizing the broader therapeutic implications of GLP-1 beyond metabolic regulation.
Collectively, GLP-1’s multifaceted interaction with its receptor across various tissues underscores its pivotal role in managing glucose homeostasis, enhancing dietary control, and sustaining overall metabolic and neurological health. By comprehending these physiological mechanisms, the full spectrum of GLP-1’s benefits can be better appreciated, informing potential therapeutic and dietary interventions.
Technological Advancements in GLP-1-Based Therapies
The discovery and synthesis of glucagon-like peptide-1 (GLP-1) analogs have marked significant milestones in medical therapeutics, particularly in the management of type 2 diabetes. The initial breakthrough came with the identification and development of Exenatide, a GLP-1 analog derived from exendin-4, a hormone found in the saliva of the Gila monster. This analog mimics the action of natural GLP-1, promoting insulin secretion and inhibiting glucagon release. Liraglutide followed as another notable development, featuring a longer half-life than Exenatide, allowing for once-daily injections. These innovations paved the way for a new class of antidiabetic medications with enhanced efficacy and safety profiles.
The creation of GLP-1 analogs presented several substantial challenges. Maintaining stability and bioavailability was paramount, as these peptides are susceptible to rapid degradation by enzymes such as dipeptidyl peptidase-4 (DPP-4). Scientists addressed these concerns by modifying the amino acid sequence of GLP-1, thereby enhancing its resistance to enzymatic breakdown. Additionally, researchers employed advanced molecular engineering techniques, including PEGylation, to extend the biological activity and stability of these analogs in the bloodstream.
Delivery methods have also evolved significantly, with subcutaneous injections serving as the primary mode of administration for many years. Although effective, the inconvenience and discomfort associated with daily or weekly injections prompted the pursuit of alternative delivery systems. Recent advancements have led to the development of oral GLP-1 formulations, such as semaglutide, which offer a more patient-friendly option while maintaining effective plasma concentrations for glucose regulation. The introduction of microencapsulation and nanoparticle delivery technologies has further improved the bioavailability and sustained release of GLP-1 analogs, enhancing patient compliance and overall treatment outcomes.
In summary, the technological advancements in GLP-1-based therapies, from the synthesis of stable analogs to innovative delivery methods, have revolutionized the management of type 2 diabetes. These innovations continue to evolve, promising even greater efficacy and ease of use for patients worldwide.
Historical Perspective on GLP-1 Research and Development
The journey of GLP-1, or glucagon-like peptide-1, began in the late 20th century. Initial research identified GLP-1 as a critical incretin hormone, chiefly involved in glucose metabolism. Scientists discovered the hormone’s ability to enhance insulin secretion in response to nutrient ingestion, shedding light on its potential in treating metabolic disorders. While the physiological role of GLP-1 in regulating blood sugar was understood, its therapeutic application gained traction in subsequent decades.
A major milestone in GLP-1 research occurred in the 1980s, when studies indicated that GLP-1 could lower blood glucose levels without inducing hypoglycemia — a significant challenge in diabetes treatment. This finding spurred a series of clinical investigations, leading to the development of GLP-1 analogs, which mimic the hormone’s functions. The early 2000s witnessed the first clinical trials of these analogs, demonstrating promising results in glucose regulation and weight management.
Technological advancements in synthesizing GLP-1 analogs facilitated their stability and prolonged activity, overcoming initial limitations like rapid degradation in the body. By the mid-2000s, the U.S. Food and Drug Administration (FDA) granted approval for the first GLP-1 receptor agonist, Exenatide, marking a pivotal point in diabetes therapy. Subsequent FDA approvals of other GLP-1-based medications, such as Liraglutide and Semaglutide, underscored their efficacy and safety, backed by robust clinical evidence.
The evolution of GLP-1 research reflects the dynamic interplay between scientific discovery and technological innovation. Noteworthy clinical studies, such as the LEADER and SUSTAIN trials, have reaffirmed the benefits of GLP-1 therapies not only in glycemic control but also in reducing cardiovascular risks, thereby expanding their clinical applications.
Today, GLP-1-based treatments are a cornerstone in diabetes management, and ongoing research continues to explore their broader therapeutic potential. Future directions include investigating novel GLP-1 analogs, combination therapies, and their implications in non-diabetic conditions. The historical trajectory of GLP-1 demonstrates a progressive refinement of our scientific understanding and therapeutic capabilities, promising novel insights and innovations in the years to come.

How can I find out more about it?
more story?
Good post. I be taught one thing more difficult on different blogs everyday. It should all the time be stimulating to learn content material from different writers and follow a bit of one thing from their store. I抎 favor to use some with the content on my blog whether you don抰 mind. Natually I抣l provide you with a hyperlink on your web blog. Thanks for sharing.