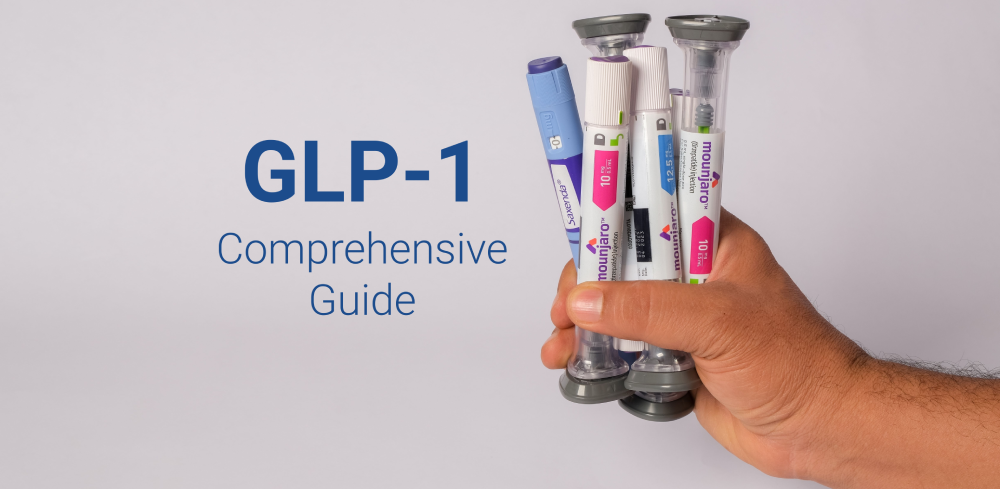
Introduction to GLP-1 Obesity Drugs
GLP-1 obesity drugs have emerged as significant players in the treatment of obesity and weight-related health issues. These medications operate by mimicking the glucagon-like peptide-1 (GLP-1) hormone, which plays a crucial role in regulating appetite and food intake. When administered, GLP-1 drugs enhance insulin secretion, inhibit glucagon release, and slow gastric emptying. This multifaceted approach helps patients achieve and maintain weight loss, addressing one of the most pressing public health challenges today.
The rising prevalence of obesity has driven an urgent need for effective treatments, and GLP-1 drugs are at the forefront of this development. Eli Lilly and Novo Nordisk are two major players in this market, offering drugs that have garnered attention for their efficacy in weight management. Eli Lilly’s drug, Mounjaro, and Novo Nordisk’s Wegovy, have shown promising results in clinical trials, leading to their approval and widespread availability. As these companies continue to innovate, the importance of GLP-1 drugs is becoming increasingly evident, particularly as healthcare systems grapple with the rising costs associated with obesity-related illnesses.
The significance of GLP-1 obesity drugs extends beyond immediate weight loss; they also contribute to the long-term management of obesity-related conditions, such as diabetes and cardiovascular diseases. The market potential for these medications is vast, fueled by both growing awareness of obesity as a chronic disease and demand for effective treatment options. As the political landscape continues to evolve, the implications for healthcare policies and market dynamics surrounding GLP-1 drugs will be vital to monitor. Understanding these factors will provide a clearer picture of the future trajectory for obesity treatments and the overall impact on public health.
Recent Earnings Reports and Market Reactions
The third-quarter earnings reports from major pharmaceutical companies, Eli Lilly and Novo Nordisk, have recently attracted considerable attention from investors and analysts alike. These reports are particularly significant as they pertain to their GLP-1 obesity drugs, which have been the focal point of market interest due to their potential impact on obesity treatment and overall revenue streams for these firms.
Eli Lilly reported earnings that fell short of market expectations, posting a revenue of $6.94 billion, which represented a year-on-year increase of just 3%. This was a stark contrast to analyst projections anticipating revenues closer to $7.3 billion. The chief factor contributing to this shortfall appears to be lower-than-expected sales of their GLP-1 drug, Mounjaro, leading to a notable shift in investor sentiment.
Political Landscape and Its Implications
The political environment plays a significant role in shaping the landscape of the pharmaceutical industry, particularly concerning emerging therapies such as GLP-1 obesity drugs. Recent developments, notably the nomination of Robert F. Kennedy Jr. as Secretary of Health and Human Services by Donald Trump, have drawn considerable attention within investor circles. Kennedy’s stance on health policy, particularly his historical skepticism regarding pharmaceuticals and vaccination programs, has raised questions about potential shifts in regulatory frameworks and funding for new drug initiatives.
Investor confidence is often swayed by perceived stability and predictability in regulatory environments. Kennedy’s appointment may introduce an element of uncertainty. While GLP-1 drugs represent a significant advancement in obesity treatment, concerns arise about whether these therapies may face increased scrutiny or shifts in approval processes under Kennedy’s leadership. Such alterations could impact not only the availability of these medications but also the extensive research and development efforts that underpin their success in clinical applications.
Moreover, the political ramifications extend beyond Kennedy’s personal views. The current administration’s broader health policy objectives could affect funding allocations and research grants, which are vital for the continued exploration of innovative treatments like GLP-1 drugs. Should there be a pivot towards more holistic or alternative treatment approaches, GLP-1 therapies, despite their efficacy, might find themselves competing for attention and resources within an evolving political context.
Ultimately, investors are weighing the long-term viability of GLP-1 obesity drugs against the backdrop of this significant political appointment. A crucial factor will be the degree to which Kennedy influences health policies, potentially shaping the trajectory and market positioning of these pharmaceuticals in an uncertain regulatory environment.
Concerns Over FDA and Generic Competition
The regulatory landscape for GLP-1 obesity drugs is ever-evolving, with the U.S. Food and Drug Administration (FDA) playing a pivotal role in shaping market dynamics. The FDA’s stringent approval process ensures that drugs meet specific safety and efficacy standards, but it also poses challenges for established manufacturers of GLP-1 medications. As new entrants seek market approval for innovative weight-loss treatments, established companies must navigate these regulatory waters carefully. The potential for competing products to gain FDA approval adds a layer of complexity, raising concerns about market saturation and price erosion.
Furthermore, the emergence of generic competitors presents additional challenges to GLP-1 drug manufacturers. As patents on original formulations expire, the influx of less expensive alternatives may undermine the pricing strategies of brand-name medications. This situation can lead to increased competition and diminished profit margins for established players, which might ultimately disincentivize further investment in the development of novel therapies. With consumers increasingly seeking cost-effective options, the pressure on the market can intensify, further complicating the landscape for GLP-1 drugs.
Another pressing issue affecting GLP-1 obesity medications is the current shortage of these drugs. The demand for effective weight-loss treatments is surging, leading to supply constraints that have not only impacted patients but have also opened avenues for knockoff treatments. These unregulated alternatives may be enticing to consumers but pose significant risks due to inconsistent formulations and a lack of rigorous testing. Established companies find themselves in a difficult position, as they must both combat these unauthorized products and ensure the steady availability of their own medications. This multifaceted competition underscores the complexities faced by stakeholders in the GLP-1 drug market, reflecting the intricate interplay of regulation, competition, and consumer demand.
Market Projections and Sales Expectations
As the market for GLP-1 obesity drugs continues to evolve, analysts have projected substantial sales expectations for major competitors in this category, particularly Eli Lilly’s Zepbound and Mounjaro, alongside Novo Nordisk’s Wegovy and Ozempic. The anticipated growth is underpinned by increasing consumer awareness of the efficacy of GLP-1 medications in managing obesity and related metabolic disorders. For instance, both Mounjaro and Zepbound have shown promising results in clinical trials, which has fueled optimism among investors and market analysts alike.
Currently, projections suggest that Zepbound could capture a significant share of the obesity treatment market, potentially rivaling platforms already established by Novo Nordisk. Analysts estimate that initial sales figures for Zepbound may reach upwards of billions of dollars within the first few years post-launch, contingent upon regulatory approvals and effective market penetration strategies. Simultaneously, Mounjaro is expected to generate consistently high sales figures as interest in GLP-1 therapies surges among healthcare providers and patients.
Conversely, there remains a level of uncertainty surrounding these projections. Factors such as regulatory changes, shifts in public perception, and wider political conditions could influence market dynamics. The recent political turbulence, notably discussions surrounding healthcare reforms, may impact funding and accessibility to these essential medications. As such, GLP-1 drugs like Ozempic and Wegovy, which are already market leaders, face potential fluctuations in their growth trajectories. Furthermore, the competitive landscape is expected to intensify as more companies enter the GLP-1 sector, which may lead to price adjustments and altered consumer preferences.
Consequently, while the projected sales for GLP-1 obesity drugs remain promising, various external factors must be monitored closely to fully understand the implications for the market. A holistic approach that considers both emerging trends and potential obstacles will be crucial for stakeholders in this rapidly changing landscape.
Rising Anti-Pharma Sentiment
In recent years, there has been a notable rise in anti-pharmaceutical sentiment among U.S. voters, reflecting deep-seated concerns regarding drug pricing, accessibility, and the ethical practices of the pharmaceutical industry. This shift in public opinion may significantly impact the market prospects for GLP-1 obesity drugs, which have emerged as a crucial treatment option for managing weight and related health issues. The increasing scrutiny of the pharmaceutical sector is a response to widespread criticism over exorbitant pricing for medications and perceived lack of transparency in the industry.
As consumers become more vocal about their grievances, policymakers are being pressured to take action, creating a challenging environment for pharmaceutical companies. The focus on reducing healthcare costs has led to greater demands for lower prices and improved accessibility to vital medications. This landscape could potentially hinder the growth of GLP-1 obesity drugs if manufacturers are unable or unwilling to meet these evolving expectations. Voter sentiment is often shaped by personal experiences and media coverage, which amplify concerns surrounding affordability and accessibility of medications.
Moreover, the complexities of healthcare policy can foster a climate of skepticism towards pharmaceutical manufacturers, particularly as discussions around healthcare reform remain contentious. In this context, the perception that companies are prioritizing profits over patient welfare may further exacerbate the negative sentiment towards GLP-1 obesity drugs. If public trust in the pharmaceutical industry continues to decline, the sales and acceptance of these treatments may be significantly impacted. Addressing these concerns will necessitate a concerted effort from the pharmaceutical sector to engage with stakeholders, promote transparency, and demonstrate a commitment to patient-centered outcomes.
Statements and Stances from Key Figures
Recent discourse surrounding GLP-1 obesity drugs has gained traction, particularly driven by statements from notable figures. Among them, Elon Musk’s remarks highlight an urgent need to address the affordability of GLP-1 inhibitors. Musk emphasized the significant financial burden these treatments place on patients, advocating for measures that would ensure wider access to these medications. His opinion reflects a growing concern regarding healthcare costs, especially when addressing obesity, a condition often exacerbated by socioeconomic factors. By prioritizing affordability, Musk’s stance could galvanize public support and potentially influence policy discussions aimed at making these therapeutic options more accessible.
Meanwhile, Robert F. Kennedy Jr. has articulated a critique of the pharmaceutical industry in relation to GLP-1 drugs. His concerns focus on the ethical ramifications of profit-driven motives within healthcare, suggesting that the current market dynamics could hinder patient-centric solutions. Kennedy’s viewpoint raises important questions about the interplay between pharmaceutical innovation and the overarching need for equitable healthcare. His stance encourages a dialogue on maintaining regulatory oversight and fostering competition, which could lead to more reasonable pricing structures for GLP-1 medications.
The remarks from both Musk and Kennedy Jr. position them at the forefront of a crucial conversation about the future of GLP-1 drugs. As public figures, their opinions hold weight and could inspire changes in legislation or corporate practices regarding drug pricing and accessibility. The synthesis of their critical perspectives underscores the multifaceted nature of the obesity treatment landscape and invites further examination of how social, economic, and ethical factors intertwine in shaping public discourse around GLP-1 inhibitors.
Investor Outlook and Market Strategies
Recent political turbulence has raised questions about the investment landscape for companies like Eli Lilly and Novo Nordisk, both key players in the development of GLP-1 obesity drugs. As governments grapple with regulatory frameworks and policy changes, investors are urged to take a nuanced approach to their decision-making. Despite potential headwinds, the long-term growth prospects for GLP-1 therapies remain strong, largely due to their effectiveness in managing obesity and related health conditions. This positive outlook is, however, tempered by ongoing market volatility, making it crucial for investors to stay informed and adaptive.
Investor sentiment has been cautious, focusing on how political uncertainties might influence public health policies and reimbursement mechanisms for GLP-1 drugs. Analysts suggest that diversifying portfolios to include various healthcare sectors may mitigate potential risks. Additionally, maintaining awareness of legislative developments will be critical, as changes may directly affect market access and pricing models of GLP-1 treatments.
Another strategy for navigating this landscape is engaging with market data and trends. Companies like Eli Lilly and Novo Nordisk may explore partnerships or collaborations that bolster their research and development efforts, enhancing their product pipelines while broadening their market reach. Investing in patient education initiatives could also create brand loyalty and drive demand, reinforcing the value proposition of GLP-1 therapies.
Moreover, strategic marketing of GLP-1 medications to healthcare providers can increase prescription rates and foster acceptance within the medical community. As the focus on obesity and its associated risks becomes more pronounced, aligning with healthcare objectives may enable companies to position their therapies favorably. In this context, careful monitoring of both political actions and market dynamics will be essential for investors looking to capitalize on the innovations in GLP-1 treatments.
The Future of GLP-1 Drugs in American Healthcare
The future of GLP-1 drugs, a critical component in the management of obesity, appears both promising and complicated against the backdrop of American healthcare. As these medications gain recognition for their effectiveness, regulatory scrutiny will likely intensify. Regulatory agencies may consider establishing more stringent guidelines for the approval and marketing of these therapies. This could lead to lengthier processes for both manufacturers and consumers, alongside increased safety monitoring. Should the government impose more regulations due to concerns related to side effects, accessibility may also suffer, impacting patients who rely on these treatments for weight management.
Public sentiment surrounding GLP-1 drugs is also evolving. As societal perceptions of obesity shift, there has been a growing recognition of the medical nature of this condition. Advocacy groups are increasingly pushing for better access to medications and comprehensive treatment strategies. This advocacy may influence policies, urging legislators to consider broader healthcare reforms that facilitate access to effective obesity drugs, including GLP-1 medications.
Technological advancements may further redefine the landscape of GLP-1 applications in treating obesity. Developments in telehealth might enable more individuals to consult healthcare professionals regarding these drugs without the barriers typically associated with in-person visits. Moreover, innovations in drug formulation may enhance the efficacy and reduce the frequency of dosing, which could improve compliance. Such advancements would not only benefit patients but also encourage wider adoption of GLP-1 drugs in obesity management strategies.
In conclusion, the trajectory of GLP-1 drugs in American healthcare is shaped by the interplay of regulatory developments, shifts in public perspective, and technological innovations. As stakeholders navigate this complex environment, the outcomes will significantly determine the accessibility and effectiveness of obesity treatments for future generations.