What is GLP-1 and Its Benefits
GLP-1, or Glucagon-Like Peptide-1, is an important hormone produced in the intestines that plays a crucial role in the regulation of blood sugar levels and appetite control. It is classified as an incretin hormone, which means it is released after eating and helps boost insulin secretion while simultaneously suppressing glucagon release, thereby contributing to better blood glucose management. The significance of GLP-1 extends beyond glucose metabolism; it also aids in slowing gastric emptying, which can contribute to a feeling of fullness following meals.
One of the primary benefits of GLP-1 is its effectiveness in supporting weight management. By promoting satiety, individuals tend to consume fewer calories, which can lead to weight loss over time. This aspect is particularly valuable for those struggling with obesity, a condition that often accompanies health issues such as type 2 diabetes and cardiovascular diseases. Research indicates that individuals treated with GLP-1 receptor agonists experience substantial weight loss, which is not only beneficial for their self-esteem but also for their overall health.
GLP-1 receptor agonists, which are synthetic versions of the human GLP-1 hormone, have gained attention in recent years. Medications like liraglutide and semaglutide have demonstrated significant positive outcomes in clinical trials, showing their ability to lower blood sugar levels effectively and reduce weight in patients with obesity and type 2 diabetes. These treatments mimic the function of natural GLP-1, providing similar benefits in appetite suppression and glycemic control. Moreover, beyond just weight management, there is evidence suggesting that GLP-1 receptor agonists may improve cardiovascular health and reduce the risk of heart-related events.
In summary, GLP-1 plays a pivotal role in regulating appetite and glucose levels, making it an essential target for therapeutic interventions aimed at managing obesity and type 2 diabetes. Increased understanding of GLP-1 underscores its potential benefits for individuals seeking to enhance their health outcomes significantly.
How to Obtain GLP-1 Medications
Acquiring GLP-1 medications necessitates a methodical approach that emphasizes medical guidance and patient suitability. The first step in this process is to consult with a healthcare provider who is knowledgeable about diabetes management and obesity treatment. These healthcare professionals can assess a patient’s overall health, existing medical conditions, and lifestyle factors to determine if GLP-1 therapy is an appropriate option.
During the consultation, the provider will evaluate criteria such as body weight, previous weight loss attempts, and other health issues, including cardiovascular health, liver function, and any cases of thyroid cancer in the family. This comprehensive evaluation is critical, as GLP-1 medications can aid in weight management and glycemic control but may not be suitable for everyone. For instance, certain individuals with a history of pancreatitis or specific endocrine disorders may need to explore alternative treatments.
If GLP-1 therapy is deemed appropriate, the healthcare provider will issue a prescription for the suitable medication. It is essential that patients obtain their prescriptions from a licensed healthcare professional who is familiar with their unique health profile. Following the prescription, individuals can acquire GLP-1 medications from local pharmacies or through reputable online pharmacies that require a valid prescription.
Moreover, patients should remain in contact with their healthcare provider after beginning GLP-1 therapy to monitor effectiveness and manage any side effects. Regular follow-up appointments facilitate adjustments in dosage or consideration of alternative therapies, ensuring optimal treatment outcomes. This ongoing engagement with healthcare professionals is crucial for achieving long-term success in weight management and overall health improvement.

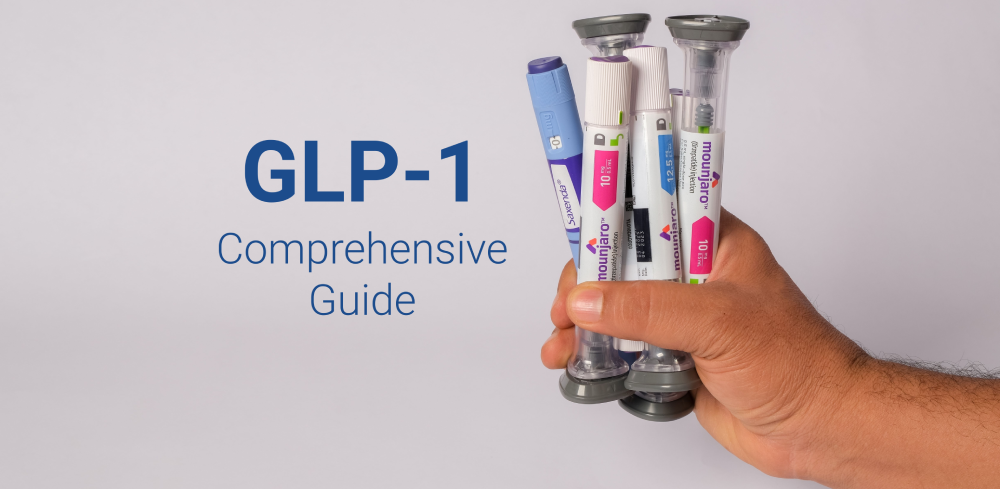
Effective GLP-1 Brands: A Closer Look
GLP-1 receptor agonists have emerged as a pivotal class of medications for managing conditions like type 2 diabetes and obesity. Among the most prominent brands in this category are Ozempic, Trulicity, and Victoza, each offering unique features and benefits while sharing similar underlying mechanisms of action. Understanding these brands is essential for individuals navigating their treatment options.
Ozempic, which contains the active ingredient semaglutide, is administered once weekly via subcutaneous injection. Clinical studies have shown that Ozempic not only aids glycemic control but also significantly promotes weight loss in patients. It has been widely recognized for its effectiveness, with some studies indicating greater reductions in HbA1c compared to other brands.
Trulicity, featuring dulaglutide as its active component, is another noteworthy GLP-1 receptor agonist. This medication is also administered weekly and boasts a user-friendly, pre-filled pen that enhances patient adherence. Like Ozempic, Trulicity has demonstrated substantial efficacy in lowering blood sugar levels and aiding weight management. Some users may prefer Trulicity for its convenience and tolerability profile.
Victoza, containing liraglutide, is distinct in that it requires daily injections. While it may seem less convenient than its weekly counterparts, Victoza has a strong clinical backing, showing robust results in lowering blood glucose levels and facilitating weight loss over longer treatment periods. Its daily administration may appeal to those who favor a more consistent routine.
When comparing these GLP-1 brands, it is essential to consider the differences in administration, potential side effects, and individual patient responses. Each medication carries its specific benefits and drawbacks, making it crucial for patients to collaborate with healthcare providers to select the most suitable option tailored to their needs. In conclusion, understanding the various GLP-1 products is key to making informed decisions about treatments available in the market.

Potential Side Effects and Considerations
GLP-1 medications, while effective for managing conditions such as type 2 diabetes and obesity, may come with a range of potential side effects. Common adverse reactions include gastrointestinal issues such as nausea, vomiting, diarrhea, and constipation. These symptoms can occur as the body adjusts to the introduction of the GLP-1 receptor agonists. Although these side effects are typically mild and transient, they can be bothersome for some patients and may lead to discontinuation of therapy if they are severe.
In addition to common side effects, there are rare but significant reactions that warrant careful monitoring. Patients may experience pancreatitis, indicated by severe abdominal pain, or signs of an allergic reaction, including rash and difficulty breathing. Hence, it is essential for individuals using GLP-1 medications to remain vigilant about their health and report any unusual symptoms to their healthcare provider promptly.
Long-term use of GLP-1 agents may also prompt additional considerations. Chronic use can raise concerns about the potential development of thyroid tumors, a risk highlighted in animal studies. Consequently, it is advisable for individuals to regularly consult with their healthcare providers, who can evaluate the benefits versus risks based on personal medical history.
Furthermore, interactions with other medications should be taken into account. Patients are encouraged to inform their healthcare providers about all medications and supplements they are taking to avoid adverse interactions. Moreover, lifestyle modifications, such as diet and exercise, can complement GLP-1 therapy, enhancing its effectiveness and promoting better overall health outcomes.