What is GLP-1?
GLP-1, or glucagon-like peptide-1, is an incretin hormone produced by the intestines in response to food intake. Its primary biological role is to enhance insulin secretion from the pancreas, which is crucial for regulating blood sugar levels. When food is consumed, GLP-1 is released, leading to an increase in insulin release, thereby promoting the uptake of glucose by cells. This action plays a vital role in maintaining optimal health and preventing elevated blood glucose levels that can lead to various health complications.
In addition to its role in insulin secretion, GLP-1 is also instrumental in appetite regulation. It influences the brain’s satiety centers, signaling feelings of fullness and thereby reducing food intake. This dual action of lowering blood sugar levels and curbing appetite contributes significantly to its potential benefits for individuals with weight-related health issues, including obesity. Since obesity is a well-known risk factor for heart disease, managing body weight through GLP-1’s appetite-regulating properties can also have a positive impact on heart health.
Moreover, GLP-1 exhibits a protective effect on the heart. Research indicates that it may improve cardiovascular health by enhancing endothelial function, decreasing inflammation, and promoting weight loss—all factors that are critical in reducing the risk of heart disease. The hormone’s interactions with other physiological mechanisms underscore its importance in blood and heart health management, suggesting that GLP-1 could be a valuable target in developing therapies for conditions like type 2 diabetes and cardiovascular diseases. Understanding GLP-1 and its multifaceted roles in the body highlights its significance as a therapeutic agent in advancing overall health.

Health Benefits of GLP-1 for Blood Conditions
GLP-1, or glucagon-like peptide-1, has emerged as a pivotal component in managing blood health, particularly concerning glucose metabolism. This incretin hormone plays a fundamental role in insulin secretion, which is crucial for regulating blood sugar levels. When glucose levels in the bloodstream rise, GLP-1 stimulates the pancreas to produce insulin, thereby aiding in the effective management of blood glucose concentrations. This process is especially beneficial for individuals with diabetes or those at risk of developing the condition.
Notably, GLP-1 has demonstrated significant implications for diabetes management by not only lowering blood sugar levels but also by mitigating the risk of associated complications. Research indicates that GLP-1 receptor agonists can lead to substantial reductions in hemoglobin A1c levels, a key marker for long-term glucose control in diabetic patients. By improving hemoglobin A1c levels, GLP-1 contributes to better overall blood health, potentially reducing the risk of diabetes-related complications such as cardiovascular disease.
Furthermore, the benefits of GLP-1 extend beyond diabetes management. Individuals with pre-diabetes may also experience positive changes in their blood glucose levels with the use of GLP-1 therapeutics. By enhancing insulin sensitivity and promoting the restoration of glucose homeostasis, GLP-1 can serve as a preventive measure against the full onset of diabetes. The reduced blood sugar levels facilitated by GLP-1 not only improve metabolic profiles but also promote cardiovascular health, a critical consideration given the relationship between blood health and heart conditions.
In summary, the role of GLP-1 in supporting blood health is multifaceted, with its ability to influence glucose metabolism, control blood sugar levels, and improve hemoglobin A1c readings showcasing its advantages for individuals with diabetes and pre-diabetes. By incorporating GLP-1 into treatment regimens, patients can experience a comprehensive approach to enhancing their blood health and overall well-being.

GLP-1 and Heart Health: A Closer Look
Recent advancements in understanding the relationship between GLP-1 (Glucagon-like peptide-1) and cardiovascular health have highlighted the potential of GLP-1 receptor agonists in mitigating heart-related ailments. These medications not only enhance glycemic control but also offer significant benefits in reducing cardiovascular risks, making them a focal point in heart disease management strategies.
Several clinical studies illustrate that GLP-1 receptor agonists can lead to notable improvements in heart function. For instance, research has shown that patients using these agents experience reduced occurrences of major adverse cardiovascular events. This can be attributed to GLP-1’s ability to improve endothelial function and promote myocardial perfusion. Enhanced blood flow supports the overall heart health, demonstrating a direct link between GLP-1 and cardiovascular benefits.
Moreover, GLP-1 plays a pivotal role in lowering blood pressure and cholesterol levels, both of which are critical factors in heart health management. By promoting weight loss and improving metabolic profiles, GLP-1 receptor agonists contribute to favorable changes in lipid metabolism, thereby reducing LDL cholesterol levels. This reduction aids in lessening the buildup of atherosclerotic plaques, further decreasing the risk of heart disease.
Additionally, there is growing evidence supporting the protective effects of GLP-1 analogs against heart failure. These medications appear to reduce the risk of hospitalization due to heart failure, highlighting their importance for patients at high risk. Enhancements in heart function, along with reductions in heart failure rates, solidify the argument for incorporating GLP-1 in comprehensive heart disease risk management strategies.
In conclusion, the integration of GLP-1 receptor agonists into treatment plans serves not only glycemic control but also significantly enhances heart health, paving the way for improved cardiovascular outcomes.
Integrating GLP-1 in a Heart-Healthy Lifestyle
Incorporating GLP-1 strategies into a heart-healthy lifestyle is paramount for individuals seeking to enhance their overall health and manage blood conditions effectively. The integration can begin with dietary considerations that favor the modulation of glucose metabolism and weight management. Consuming a balanced diet rich in whole grains, lean proteins, healthy fats, and a variety of fruits and vegetables can promote heart health, reduce systemic inflammation, and ultimately improve one’s health profile.
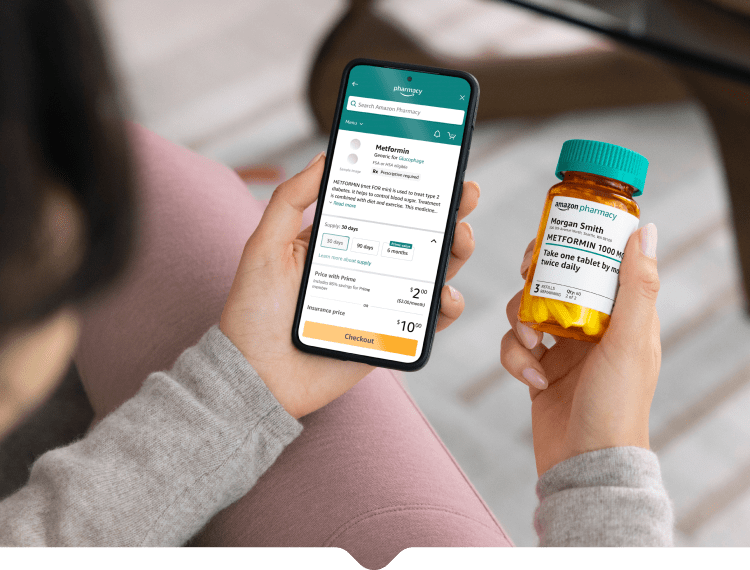
GLP-1 receptor agonists, a class of medications designed to mimic the effects of the naturally occurring GLP-1 hormone, can be invaluable tools in managing blood sugar levels and promoting weight loss. These medications have demonstrated a positive impact on cardiovascular health, thereby serving an important role in the treatment plans for individuals with diabetes and existing heart conditions. However, it’s essential for patients to engage in a collaborative approach with their healthcare providers to tailor any medication regimen to their specific health needs and goals.
In addition to dietary adjustments, regular physical activity is crucial in creating a comprehensive wellness strategy. Engaging in moderate-intensity exercises, such as brisk walking or cycling, can significantly improve cardiovascular fitness and enhance the body’s response to insulin. Furthermore, stress management techniques, such as mindfulness and yoga, can augment the health benefits of a heart-focused lifestyle.
Recent developments in GLP-1 research continue to reveal exciting possibilities in the realm of metabolic and heart health. As scientists uncover the multi-faceted roles of GLP-1 hormones, individuals can look forward to an evolving landscape of health strategies designed to promote optimal well-being. In conclusion, by combining lifestyle changes, medical treatment with GLP-1 medications, and ongoing communication with healthcare professionals, individuals can pave the way toward a healthier heart and robust blood health.